Eye care professionals are always searching for ways to improve treatment options for eye diseases. Recently, a tonometer has brought a significant breakthrough in the field. The small instrument measures eye pressure (IOP) to detect eye diseases like glaucoma.
This guide provides information about handheld tonometers, their applications, and how to choose the right device.
The Importance of Eye Pressure
The importance of intraocular pressure (IOP) to eye health cannot be overemphasized. A balance between aqueous humor production and drainage maintains it and determines IOP. Typically, IOP readings range from 10 to 21 mmHg, but they vary throughout the day.
High eye pressure is a risk factor for glaucoma, which can harm the optic nerve and cause vision loss if not treated. Regular monitoring of IOP is essential for the early detection, diagnosis, and management of glaucoma and other ocular disorders.
What Is a Handheld Tonometer?
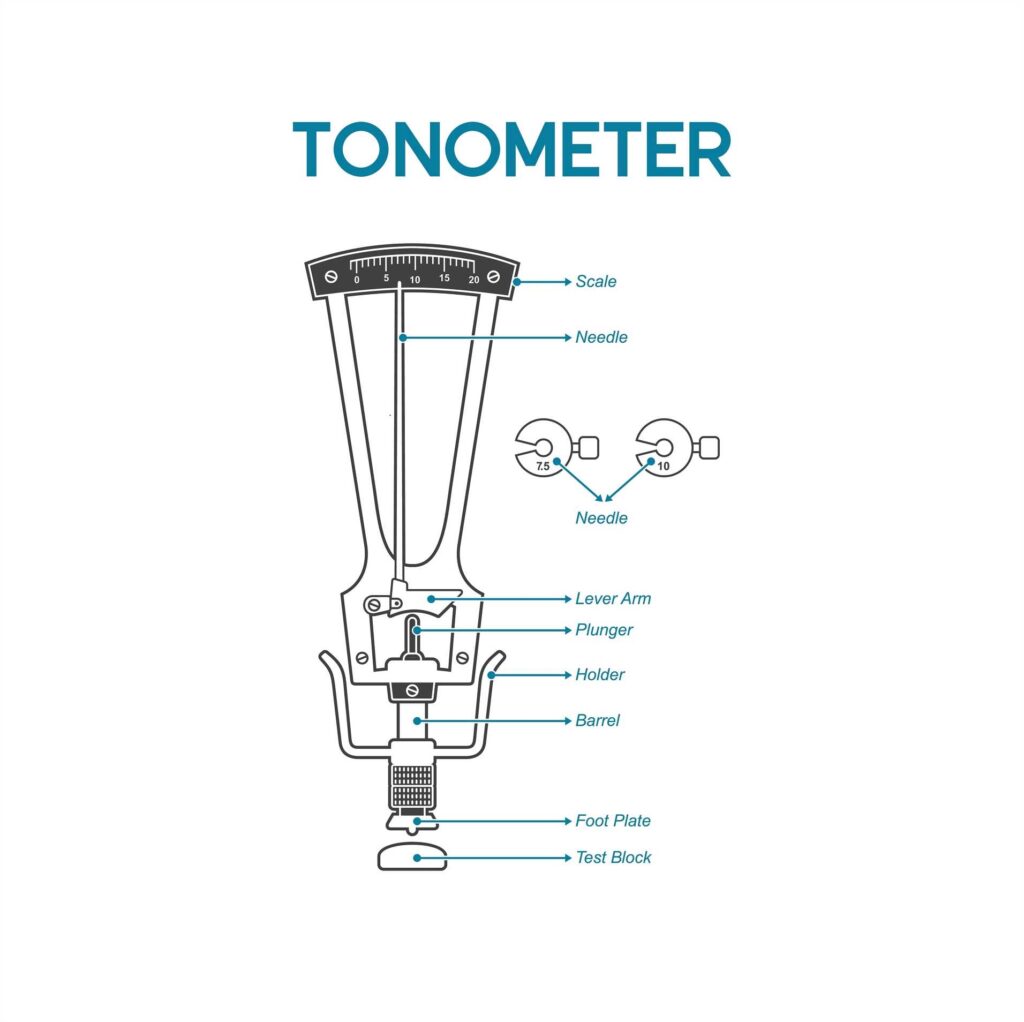
A handheld tonometer measures intraocular pressure quickly and accurately while being portable. This distinguishes it from traditional tonometers because it easily enables the measurement of IOP in different locations. You can use them in clinical practices, practices, or remote locations. Handheld tonometers use different methods to measure IOP.
Advantages of Handheld Tonometers
Each type of handheld tonometer has its advantages.
Portability and Flexibility
Handheld tonometers are portable, making them easy to take to different examination rooms, clinics, and remote locations. This flexibility allows screenings and examinations in various settings, such as nursing homes, schools, and community health centers.
Efficiency and Time Savings
Many handheld tonometers are designed to be user-friendly, requiring minimal training and setup time. This can increase efficiency and reduce examination time. Rapid IOP measurements can speed up patient flow and optimize clinic operations.
Versatility and Adaptability
Doctors can use handheld tonometers in various patient positions. This makes examining individuals with mobility issues easier, helps those with difficulty positioning themselves for traditional tonometry, and can improve patient comfort.
Expanded Access to Care
Handheld tonometers improve access to eye care services by enabling IOP measurements in settings beyond traditional clinics. This is particularly beneficial for underserved populations and individuals in remote areas.
Patient Comfort and Acceptance
Certain handheld tonometers, like non-contact models, improve patient comfort by not requiring contact with the cornea. This can also reduce anxiety.
This can be especially important for pediatric patients or those with sensitive eyes.
Integration into Telemedicine
Handheld tonometers can be integrated into telemedicine, making remote IOP monitoring and consultations possible. This is valuable for patients with limited mobility or remote areas.
Types of Handheld Tonometers

There are many kinds of tonometers on the market, each with distinct features and uses.
Goldmann Applanation Tonometry (GAT)
Doctors consider the Goldmann Applanation Tonometer the gold standard for measuring IOP. This process flattens a specific part of the eye’s surface with a set amount of pressure. It then measures eye pressure based on that pressure. GAT gives precise results but needs specialized equipment and skills, making it less practical in some situations.
Rebound Tonometers
Rebound tonometers employ a probe that briefly touches the cornea. They gauge IOP by measuring how the probe slows when it hits the eye’s surface. These tonometers are user-friendly and do not require anesthetic eye drops.
Applanation Tonometers
Applanation tonometers utilize a probe tip to touch the cornea and provide digital IOP measurements. Doctors can use them on patients with irregular corneas or those who wear contact lenses. While they generally offer accuracy, they may require an anesthetic.
Non-contact Tonometers
Specific handheld devices utilize air puff technology to measure IOP without touching the eye. Although these devices are typically more comfortable for patients, contact methods may need to be more accurate.
How to Use a Handheld Tonometer

To use a handheld tonometer effectively, here are some general tips:
- Prepare the device: Calibrate the tonometer daily and use new, sterile disposable tips for each patient.
- Position the patient: Have them seated or reclined comfortably, with their head stable.
- Anesthetize the eye: Apply topical anesthetic drops for contact tonometers to the patient’s eye.
- Hold the tonometer like a pencil, keeping it parallel to the floor and about half an inch away from the cornea.
- Take measurements: Gently touch the tonometer tip to the center of the cornea several times.
- Most devices will signal when they have taken sufficient measurements to calculate an average IOP.
- Repeat if necessary: Take multiple readings to ensure accuracy and consistency.
- Record and interpret: Document and evaluate the results in the context of the patient’s overall ocular health.
By following these steps, it is possible to get accurate IOP measurements while ensuring patient comfort and safety.
Choosing the Right-Handheld Tonometer

Selecting the optimal handheld tonometer involves a thorough evaluation of several key factors.
Accuracy and reliability:
- Only use tonometers with clinical studies demonstrating their accuracy and reliability compared to the Goldmann application tonometer (GAT).
- Make sure that the tonometer can accurately measure a wide range of IOP values, from regular to high.
- Consistent IOP measurements across multiple readings and users are essential for accurate diagnosis and monitoring.
Ease of use and efficiency:
- A user-friendly interface with clear instructions and minimal setup time can improve workflow efficiency.
- Consider the time and resources needed to train staff on proper tonometer use.
- Some tonometers offer built-in data management or connectivity options for seamless integration with electronic health records (EHRs).
Consider patient comfort:
- Non-contact tonometers may be more comfortable for patients, especially children or those with sensitive eyes.
- Shorter examination times can improve patient satisfaction and reduce anxiety.
- Consider patient preferences and experiences when determining which tonometer to use.
Versatility and adaptability:
- Evaluate the tonometer’s suitability for different patient demographics, including infants, children, the elderly, and those with specific eye conditions (e.g., dry eye, corneal diseases).
- Determine if the tonometer is suitable for your practice’s specific needs. This includes screening for glaucoma, postoperative care, and telemedicine.
- Consider the tonometer’s performance in different lighting conditions and temperatures.
Cost-effectiveness:
- Compare the upfront cost of different tonometer models.
- Factor in the cost of consumables (e.g., disposable tips, batteries) and maintenance.
- Evaluate the potential cost savings and increased efficiency associated with each tonometer.
Look for portable and durable devices:
- Consider the tonometer’s size and weight for easy transportation.
- Adequate battery life is essential for extended use without interruptions.
- The tonometer should be durable enough to withstand the demands of a busy clinical environment.
To find the best handheld tonometer for your practice and patients, consider these factors and compare different options. This will help you make an informed decision.
Comparing Popular Handheld Tonometers
Here’s a comparison of some widely used handheld tonometer models:
Icare ic100 ($1,950.00)
Technology: Rebound tonometry
Pros:
- No need for anesthetic. This makes it more comfortable for patients and quicker for clinicians.
- Easy to use. The device is user-friendly, requiring minimal training to operate effectively.
- Suitable for children and uncooperative patients. Its non-invasive nature makes it ideal for pediatric and difficult-to-manage patients.
- Relatively inexpensive. It is budget-friendly compared to some other handheld devices.
Cons:
- IOP may be slightly underestimated compared to Goldmann application tonometry. If not calibrated or interpreted correctly, this can lead to underdiagnosis.
- Corneal thickness and curvature can affect accuracy, and changes in the cornea can impact readings. The clinician must carefully consider these factors.
- Generally, it is more budget-friendly than other handheld tonometers.
Tono-Pen AVIA Tonometer ($1,590.00)
The Reichert Tono-Pen AVIA Handheld Tonometer is a reliable and convenient tool for measuring intraocular pressure. Its ease of use, portability, and accuracy make it an excellent choice for eye care professionals in various settings. However, cost, training, and maintenance considerations are essential to ensure its effective and accurate use.
Technology: Applanation/indentation hybrid
Pros:
- Versatile: Can be used on various corneal conditions, including irregular corneas.
- Provides statistical confidence indicator: This helps ensure the reliability of the measurements.
- Relatively accurate: Offers dependable readings when used correctly.
Cons:
- Requires disposable tip covers: Adds to the ongoing costs and necessitates regular supply management.
- Multiple readings may be needed for accuracy. This can take time, but it is necessary to obtain a reliable measurement.
- Higher cost compared to other models: This can be a consideration for budget-conscious practices.
- Mid-range pricing.
Reichert PT100 Portable Non-Contact Tonometer
Technology: Air-puff, non-contact
Pros:
- No corneal contact: Reduces the risk of infection and is more comfortable for patients.
- Comfortable for patients: The non-invasive nature is less intimidating and more comfortable.
- No risk of cross-contamination: Eliminates the need for disposable covers and reduces the risk of transmitting infections.
Cons:
- Bulkier than other handheld models: This can make it inconvenient to use in specific settings.
- In some cases, the results may not be as accurate, especially for patients with issues with their corneas. The corneal structure can impact readings.
- Typically higher priced due to the advanced technology involved.
Diaton Transpalpebral Tonometer
Technology: Through-the-eyelid tonometry
Pros:
- No corneal contact: This suits patients with corneal issues or those wearing bandage contact lenses.
- Can be used over bandage contact lenses: Adds versatility in specific clinical situations.
Cons:
- Requires more skill to obtain accurate readings: The technique is less intuitive and requires training.
- May be less precise than direct methods: This can impact the reliability of the readings.
- Researchers are still studying and validating the effectiveness of relatively new technology with limited data on long-term accuracy.
- Often more of a premium price point.
Reichert Tono-Vera Tonometer
The Reichert Tono-Vera Tonometer is a portable device with advanced technology that allows eye care professionals to quickly and accurately measure intraocular pressure. Despite its benefits like ease of use and cleanliness, consider a product’s cost and upkeep to ensure it meets your needs.
Technology: It ensures proper positioning and alignment for accurate readings. It is lightweight and user-friendly, allowing for comfortable handling and operation.
Pros
- This device’s handheld design makes it easy to carry and use. You can take it with you to clinics and hospitals and during field visits.
- Accuracy: The active alignment and positioning sensor technologies provide highly accurate IOP measurements.
- Ease of Use: Easy to use with clear instructions for all users, whether experienced or new.
- Hygiene: Disposable probes ensure high hygiene standards and reduce the risk of cross-contamination between patients.
- Patient Comfort: The quick and gentle measurement process enhances patient comfort and compliance.
- Versatility: Suitable for many patients, including those with corneal irregularities.
Cons
- Cost: The initial investment and ongoing cost of disposable probes can be higher than traditional tonometry methods.
- New users may need some time to understand how things work and begin to see positive outcomes. They might also take a while to get comfortable with the easy learning curve, become accustomed to the system, and consistently achieve optimal accuracy.
- This device runs on battery power, which requires regular charging. This can be a problem in places with limited access to electricity.
- Durability: Handheld devices may be more prone to damage from drops or mishandling than stationary equipment.
- Limited Features: The device is suitable for measuring IOP. However, it may not have all the additional diagnostic features in other ophthalmic devices.
iCare IC200 rebound tonometer ($1,625.00)
The iCare IC200 Tonometer is a modern device that accurately measures eye pressure without being invasive, which provides comfort for patients.
Its ease of use, versatility, and hygienic design make it a valuable tool for eye care professionals. When choosing a product for a specific practice, consider cost, battery usage, and training needs.
Technology: measures eye pressure by detecting the movement of a small probe that briefly touches the cornea. It can be used in different positions, such as sitting, lying down, or standing. It also has an automatic measuring sequence for accurate results.
Pros
- Non-Invasive: The rebound technology provides a gentle, non-invasive method for IOP measurement, enhancing patient comfort.
- The interface is simple and easy to use. Automated systems take the measurements. This makes it easy for all users. It doesn’t matter if they are new or experienced.
- Versatile Positioning: The ability to measure IOP in various patient positions increases its versatility in different clinical settings.
- No Anesthetic Required: Eliminates the need for anesthetic drops, saving time and reducing patient discomfort.
- Hygiene: Using disposable probes ensures high hygiene standards and reduces the risk of cross-contamination.
- Portability: Lightweight and handheld design allows for easy transport and use in multiple locations.
Cons
- Price: Using disposable probes for tonometry may cost more initially and over time than some traditional methods.
- Battery Dependency: Needs frequent charging and upkeep of batteries, which can be challenging in places with limited power.
- Handheld devices are more likely to sustain damage from drops or mishandling because of their durability.
- The readings may vary if you do not position the probe correctly. Proper training is necessary for achieving the best results, even though they are typically accurate.
- Limited Features: Primarily designed for IOP measurement, it may lack additional diagnostic features in more comprehensive ophthalmic devices.
iCare HOME2 Tonometer ($1,155.00)
The iCare HOME2 Tonometer allows patients to monitor their eye pressure at home, helping them take a more active role in managing their eye health. Its user-friendly design, noninvasive nature, and convenience make it an attractive option for many. However, considerations regarding cost, training, and technology reliance are essential to ensure effective and accurate use.
Technology: It uses a small, lightweight probe that momentarily touches the cornea to measure IOP. It features an intuitive interface with clear instructions, suitable for non-professional use. It also includes automated sequences to ensure consistent and accurate measurements.
Pros
- Convenience: Allows patients to monitor their IOP at home, reducing the need for frequent clinic visits.
- Non-Invasive: Gentle, rebound technology is comfortable and does not require anesthetic drops.
- User-Friendly: Designed for easy use by patients, with clear instructions and automated measurements.
- Frequent Monitoring: Regular monitoring can lead to better management of glaucoma and other conditions.
- Wireless Data Transfer: Facilitates communication between patients and eye care professionals for timely adjustments in treatment.
- Hygiene: Disposable probes ensure high standards of hygiene and prevent cross-contamination.
- Data Storage: The ability to store multiple readings allows for comprehensive tracking of IOP trends.
Cons
- Cost: The device and ongoing cost of disposable probes can be significant for patients.
- Training Required: Patients must be adequately trained to use the device correctly, which can be a barrier for some.
- Battery Dependency: Requires regular charging and maintenance, which can be a limitation for some users.
- The device’s accuracy can vary if it is not used correctly. Training and practice are essential to get accurate readings.
- Limited Features: Primarily focused on IOP measurement, lacking additional diagnostic capabilities in clinical devices.
- Technology Reliance: Dependence on wireless connectivity for data transfer may be an issue in areas with poor internet access.
Key Considerations When Choosing a Handheld Tonometer

Here are some key elements to consider when choosing which handheld tonometer to use:
- Accuracy: However, the applanation and hybrid models offer relative precision compared to other handheld tonometers.
- Ease of use: Do this while you are learning and to obtain results that are consistent with the patient’s needs.
- Patient comfort: Some patients may prefer non-contact or through-the-eyelid alternatives.
- Costs: Balancing upfront costs with ongoing consumable costs (e.g., tip covers).
- Portability: Is there a weight limit? How big is the device?
- Clinical needs: Does it have features that meet your specific population and practice requirements?
- Watch for updates on handheld tonometry technology, like advancements in artificial intelligence or improved image processing capabilities.
- Clinical supporting data: The priority should be on clinical support data for the accuracy and reliability of devices.
- Training users properly will maximize the performance of all handheld tonometers.
Eye care practitioners can choose the best handheld tonometer for their practice and clients by carefully considering these factors.
Accuracy and Best Practices
While handheld tonometers offer numerous advantages, some may slightly underestimate IOP compared to traditional Goldmann application tonometry.
To get the most accurate results:
- Take multiple measurements and average the results.
- Do regular calibrations according to the manufacturer’s recommendations.
- Be aware of factors affecting IOP readings, such as corneal thickness, time of day, and the patient’s position.
- Confirm unusual or clinically significant readings with Goldmann application tonometry whenever possible.
- Keep up to date on the latest research regarding the accuracy of different Tonometers.
Integrating Handheld Tonometers into a Clinical Practice
Incorporating handheld tonometers into a practice can significantly increase efficiency and improve patient care. These devices are handy for:
- Quick IOP checks during follow-up visits
- Screening events and community outreach programs
- Home visits for patients with mobility issues
- Pediatric examinations
- Emergency or after-hours care
Eye care professionals can improve their diagnoses by using handheld tonometers. They can also provide better care to patients. This is in addition to traditional methods.
Future Trends in Handheld Tonometry
Handheld tonometry is expected to see more advancements as technology progresses. Anticipated developments include:
- Enhanced precision achieved through algorithms and sensor technology
- Integration with applications for analyzing data and monitoring patients
- All-in-one devices capable of conducting various diagnostic tests using a single handheld tool
- Improved connectivity features facilitating smooth integration with practice management systems
Staying updated on these emerging technologies is crucial for delivering optimal patient care.
Handheld tonometers have improved eye care by providing efficient and patient-friendly pressure (IOP) measurements. Their versatility and adaptability make them valuable across a range of scenarios.
When choosing a device, consider factors like accuracy, ease of use, and patient needs despite the benefits they offer. Incorporating handheld tonometers into eye examinations can enhance diagnostic capabilities and patient outcomes and aid in the early detection of eye diseases.

Be First to Comment